Navigating Motherhood -
Insecurities and Fears For New Moms
FEEDING CHALLENGES
Hey there, amazing moms!
Motherhood is a beautiful journey, filled with love and unforgettable moments. In our last chat, we tackled the sometimes-overlooked Mom Guilt. Now, in our ongoing series on Navigating Motherhood – Insecurities and Fears For New Moms, let’s dive into another part of this beautiful adventure – feeding.
Breastfeeding can be a magical connection between you and your little one, but it isn’t the only way that is utilized to help nourish your baby. In this blog, we’re focusing on common feeding issues that many moms face and sharing some tips on how to overcome them, from breast to bottle to tube feeding, and then transitioning into solid foods. Whether you’re an expecting mom getting ready for the journey or a new mom looking for some guidance, we’re here to support you and provide solutions for your child’s feeding concerns.
Common Feeding Challenges and Solutions:
Latching Difficulties: This can occur when a baby attempts to attach or latch onto their mother’s breast during breastfeeding. A successful latch is crucial for effective breastfeeding, as it ensures that the baby can properly access and extract milk from the breast. Latching difficulties can arise for various reasons, and they can be a source of frustration and discomfort for both the baby and the breastfeeding mother. Here are some common issues related to latching difficulties and their explanations:

- Tongue or Lip Tie: A tongue tie occurs when a piece of skin beneath the baby’s tongue (the lingual frenulum) or lip restricts its movement. This can make it difficult for the baby to latch and effectively feed. This can be assessed by a pediatrician, pediatric dentist, lactation consultant (IBCLC), or a speech, occupational, or physical therapist who specializes in feeding therapy. These lip and tongue ties can play into overall body tightness and discomfort, leading to issues with shoulder and neck tightness, torticollis, and straining while feeding. Sometimes these are easy to spot, but other times need multiple specialists to confirm a diagnosis. A severe lip or tongue tie may require surgical intervention, others possibly just stretching and/or bodywork.
- Positioning Issues: Incorrect positioning of the baby at the breast can lead to latching problems. A poor latch may result from the baby not being aligned properly with the nipple (this could be at the head/neck, arms or legs).
Addressing latching difficulties often involves seeking support and guidance from a lactation consultant or feeding therapist. These professionals can help identify the specific issue causing the latching problem and provide guidance on how to correct it. Solutions may include adjusting the baby’s positioning, ensuring a deep latch, and addressing any anatomical or medical factors contributing to the difficulty. Proper latching is vital for efficient breastfeeding, ensuring the baby gets enough milk and preventing nipple discomfort for the mother.
Be sure to support your baby in a way that their chin is tucked close to their chest, both of their hands can cup the breast and their knees are above their hips. This is called ‘promoting midline’ and is incredibly helpful for babies to help stay regulated and focus on the only thing they need to: feeding, rather than wondering where their head, arms or legs are in space. This can prevent unnecessary repositioning as well. Proper positioning during feeding is a game-changer. It not only prevents discomfort and eventual postural disturbances for you, the amazing mom, but also supports your baby’s motor skills and development.
Make sure you’re in an upright and comfortable position, with support behind your back, under your arms and lap, and that your baby is well-supported. If you can’t see your baby well, consider tucking additional pillows under them so that you don’t need to strain your neck to watch them. Encourage them to bring their hands to midline (rather than allowing the hands to drop behind your ribcage or under your arm) and work on that chin tuck (instead of letting their head fall backwards over your elbow) – these motor skills are essential for play and positioning outside of feeding. Even just by placing their hands on the breast or bottle passively, it helps keep your baby calm and learn that they have hands, and what their hands can be used for. This will lead to them bringing a pacifier or teether to their own mouth when upset or teething, and save you a trip to their crib in the middle of the night (and who doesn’t want that?).
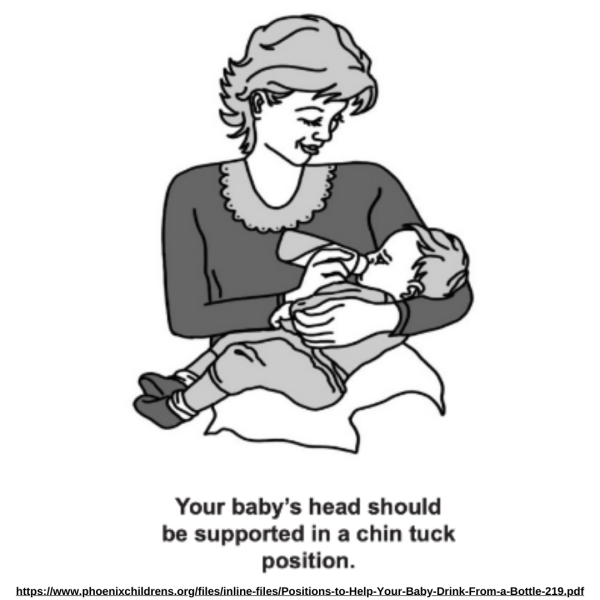
They make excellent supportive pillows to aid in this positioning, and our favorite is the boppy pillow, or a variation of sorts. Here are some links to guide you, that promote hands to midline and a thin tuck position, like how the mom above is feeding her baby: Nursing Pillow and Boppy pillow (we’re partial to this one because it can be used for motor development later on).
Reflux: Reflux, or GERD, occurs when there is regurgitation of the liquid from the stomach to the esophagus. Sometimes reflux can be silent, staying inside of the esophagus, other times it can be quite visible, and best described as frequent or excessive ‘spit up.’ Reflux can happen due to pressure on the stomach and intestines after eating, a poor closure of the sphincter between the stomach and the esophagus or a chemical reaction, possibly due to some sort of ingredient intolerance or allergy. If your baby is experiencing reflux, they may employ a few tactics to prevent the extremely unpleasant feeling of heartburn from happening. Commonly seen compensations include tilting their head to the side (possibly leading to torticollis); arching; clenching or straining at their neck, shoulders, abdomen and hips; refusal to eat; tummy time avoidance/ tummy time intolerance, leading to more time on their back and a flat head (plagiocephaly) and possibly a baby helmet (DOC band). The less our babies move, the harder it is to gain strength and learn how to use their muscles. This leads to overall delays and can also lead to difficulties with reflex integration (when their movements appear choppy and involuntary). Note, if your child is already experiencing any of these symptoms, contact us immediately for a free consultation, as M&G treats these conditions on a daily basis. Other commonly seen side effects with reflux include constipation, vomiting, burping, wheezing, choking, lack of weight gain (failure to thrive) and bumpy or irritated skin (eczema). If your baby suffers from reflux, there are natural and medical treatment options that you can discuss with your pediatrician.
Related to their motor development, it is important to give them at least 30 minutes of rest between finishing their feed and placing them in tummy time. Consider doing gentle infant massage and basic stretches to prevent them from developing tightness as a compensatory pattern. Tight babies tend to be delayed with head control and tummy time tolerance, which leads to struggles with rolling back to tummy, crossing one hand to the other side to grab toys (midline) and crawling. These lead to difficulties and frustration with their play, which in turn leads to even more mom guilt.
Bottle feeding: There are many types of bottles, nipples, and flow rates that exist. Babies go through different stages and phases of what will work best for them to get their nutrients through a nipple. If your baby often chokes, coughs or gags during bottle feeds, this could be a sign that the flow rate is too quick, either due to the mother’s breast milk letdown, or the flow rate of the nipple. Many moms who end up bottle feeding just choose to poke holes in the nipple if baby starts to struggle to get the breastmilk or formula out, but be advised that this is not recommended, and is a huge risk factor for the baby to choke. Look at the size of the nipple and consider ordering the next size up instead. Bottle feeding can be done for breast milk, formula or cow’s milk (based on your child’s pediatrician’s recommendation). If you or baby has a hard time with breast feeding, bottle feeding a is a great alternative. Don’t give up hope if you try a few and they don’t stick! A feeding therapist or IBCLC is a great resource if you start to feel stuck with this decision (hint: we’ve already provided you with several)!
NG Tubes and G Tubes: Sometimes, babies might have medical conditions or issues that make it necessary to use NG (Nasogastric) tubes or G (Gastrostomy) tubes for feeding. These tubes ensure they get the nourishment they need to grow and thrive. If your baby needs this support, don’t worry; there are specialists who can help you navigate this journey. Be sure to not discontinue use of these or change the amount of thickener added to your baby’s intake without advice from your child’s GI (gastrointestinal) specialist.
Eating Solids: When your baby starts to become older, stronger and longer, consider placing them in a more upright position when they drink out of their bottle and when they are starting solid foods. Solid food (purees or thicker) transitions from the bottle can be exciting, but also an incredibly stressful time. Comparing to your friend’s or family’s kids who are ‘eating everything in front of them’ can often lead to a reclusive lifestyle if your baby isn’t there yet. And baby led weaning isn’t appropriate for every child, particularly if they don’t have the appropriate suck/swallow/breathe pattern, they have a lip or tongue tie, or struggle with keeping food down. Remember that some choking is a normal part of learning how to eat solids. The best thing that you can do to ensure that your baby is ready for solids is wait until they have head control (they can hold their head up on their own when you’re only supporting at the waist). If you or someone else would still refer to them as having a ‘bobble head,’ or they can only hold their head upright for a few seconds, it’s too early. This transition happens between 4-7 months in a typically developing child. If your baby is past this age and you’re concerned about them holding their head up, this is your sign to schedule a free consultation with M&G. The next best thing you can do to prepare for a baby’s positive transition from liquids to solids is to invest in supportive seating.

High chairs with adjustable footrests can be incredibly helpful when considering seating for baby, because it will last, saving you hundreds of dollars and tons of space in the long run. Not only can it grow with your baby, but it promotes upright posture that helps with motor skill development necessary for utensil use, playing with their hands, and coordination hands together later on in their development. If you need more convincing, check out this article.
Although tempting, the high chairs that are transportable and can easily be placed or hung on the end of a table are generally insufficient in providing any baby or toddler a firm, supportive surface to ensure ease with feeding. We personally do not recommend use of these. If necessary to use in certain situations, add in additional pillows or blankets for full back and head support, support under their elbows and forearms so their hands can easily rest on the table in front of them, and push something under their feet so they have a footrest (90/90/90 positioning); this will also prevent tantruming due to discomfort 10-15 minutes into mealtime and allow for more family bonding (or time for you to have hands free during mealtime).
Whatever you do, don’t purchase the bumbo chair, and if you were already gifted this, place it in the nearest garbage bin. Seats that are heavily rounded at the bottom promote a rounded pelvis, also known as a posterior pelvic tilt. This allows the abdominal muscles to ‘rest’ and promotes forward head and rounded shoulder posture. Practice makes permanent, so if you want your baby to have good posture, do them a favor and don’t use it! The other detriment to the bumbo is that it doesn’t allow for foot contact, forcing the baby to lean back into the seat or lean heavily to the side, which could eventually lead to tightness in the muscles, which then pull on the bones in the spine, leading to scoliosis. Finally, there is no tray for them to rest their arms on, also leading to arm fatigue or disuse when eating.

Empowerment Through Knowledge
Although M&G is not a corporation that specializes in feeding therapy, we have aimed to support you on this topic based on how it relates to mom guilt. If you are experiencing mom guilt related to breastfeeding, bottle feeding or transitioning to solid foods for your little, at the end of this article, we’ve provided you with highly recommended, reliable and confidential resources to get you the support that you need to keep you going as the best mom you can be!
Once they are meeting their nutritional needs, your baby will have the energy to perform motor skills and catch up on their milestones (head control, tummy time tolerance, sitting, crawling, standing, walking, running, jumping, ball play…). Many kids who have difficulties with their feeding skills tend to have poor body awareness and core strength, which is what could potentially lead you to needing pediatric physical therapy. By addressing potential tongue and lip ties and postural alignment early on, you can prevent the need for physical therapy later on. We care about you and about preventing pediatric physical therapy, so take this knowledge and pass it along to other mamas, so we can keep your babies healthy, strong and happy, and keep your mom guilt to a minimum.
At the heart of this blog is the belief that knowledge is a powerful tool for empowerment. We want to equip you with the information, strategies, and support you need to overcome feeding challenges, so you can continue to provide your baby with the nourishment, comfort, and bonding that breastfeeding offers.
Agave Peds: Dr. Agarwal is a pediatrician, and Dr. Bower is a pediatric dentist, who surgically release tongue and lip ties: www.tonguetiekids.com and https://www.ashleebowerdmd.com
Eat Play Grow Kids: Ms. Meredith is a speech therapist who specializes in feeding from infants through older children, based out of the East valley: www.Eatplaygrowkids.com More Than Words: Ms. Kalee is the owner, a speech therapist who specializes in feeding and also offers lactation consulting services throughout the valley: www.breastfeedingsupportsolutions.com
Phoenix Feeding Therapy: Ms. Meghan is the owner, a speech therapist, who specializes in feeding therapy near midtown Phoenix. www.phoenixfeedingtherapy.com More than a Latch: Ms. Kylie specializes in pregnancy dietetics and is also a lactation consultant, based out of the East valley: Www.Morethanalatch.com
AZ Breastfed babies: Ms. Amey is a lactation consultant and has several others working on her team. She offers a support group for you to meet other mamas at The Motherhood Co, as well as in home and virtual consultations. www.azbreastfedbabies.com
Growing Forward Therapy: Ms. Chelsea is an occupational therapist who performs body work related to overall tightness with lip/tongue ties. www.growingforwardtherapy.com Arizona NICU grads: Ms. Dee and Ms. Rama are occupational and feeding therapists and can help with feeding concerns. www.nicugrads.com
Feeding Matters: An organization that offers helpful support online.
Feeding Littles: A highly entertaining and helpful insight into how to help transition into solids and allow toddlers to get more enjoyment out of mealtime, performed with real-life acting by Ms. Megan & Ms. Judy.
Freeze dry your breast milk, for under or overproduction, with some of the best: Www.boobiejuice.com or www.milkbymom.com
As you’ve now learned, there’s no one-size-fits-all solution, and your baby’s well-being is what matters most. Remember, you’re doing an incredible job as a mom, and there’s a whole community of experts and support ready to assist you every step of the way!
See you on the next blog, where we’ll dive even deeper into the wonderful world of motherhood!
