Commonly Treated Conditions
Whether your child has a confirmed or suspected condition, we're here to help you, every step of the way.
When seeking physical or occupational therapy for your child, it’s important to choose a pediatric therapist.
Pediatric physical and occupational therapists understand developmental milestones and how to motivate children through fun, play-based interventions.
Below are our most commonly treated conditions, though we’re familiar with many others—feel free to contact us to discuss your child’s specific needs.
(Global) Developmental Delay
Developmental delay indicates that a child is not meeting their milestones on time. Generally, PT and OT work on 'motor' delays. If a child has global developmental delay, they may also benefit from additional therapies and specialists. Be sure to check out AZEIP (early intervention) if your child has this condition in order to receive free, in home services before they turn 3 years old. Our PT and OT services are a great additional support or alternative if you wish to opt-out of AZEIP.
Torticollis (wry neck)
Torticollis (pronounced tort-ih-call-is) is a condition in which the neck has asymmetry and is tilted in one direction and rotated in the opposite direction. This is hard to initially see, but easy to identify by looking through past photos of your little one and noticing they are constantly tilting their head in one direction (like they're a model). They have difficulty looking the other direction and demonstrate a hand preference prior to 2-3 years old as a result, making activities that require looking to both sides or using both hands in bimanual tasks difficult.
Plagiocephaly/ Brachycephaly/ Scaphocephaly
Plagiocephaly is a condition in which there is asymmetry in the skull bones. Generally, you'll see that the eye, cheek and lips appear bigger, more 'full' or more elevated on one side of the face. The face may appear to be 'flattened' on the other side. If one side of the forehead or skull is pushing out, this is referred to as 'bossing.' Brachycephaly (pronounced brack-ee-sef-aly) is when the skull is much more flat in the back. Scaphocephaly (pronounced skaf-ee-sef-aly) is defined as the head being longer and thinner than average. Many individuals choose to utilize PT or OT for these conditions to prevent use of a DOC band (helmet). If a helmet is needed, it can be kept on during these therapy visits while the therapist addresses the other areas of concern, such as torticollis.
Macrocephaly (larger than normal head)
Macrocephaly is a condition in which the head is larger than average, or >97% for their age and sex.
Microcephaly (smaller than normal head)
Microcephaly is a condition in which the head is smaller than average, or >2 standard deviations for their age and sex. It is often associated with learning difficulties and brain abnormalities.
Hydrocephalus
Hydrocephalus is a condition in which there is extra fluid in the brain. This is often associated with macrocephaly due to the extra pressure of the fluid on the brain.


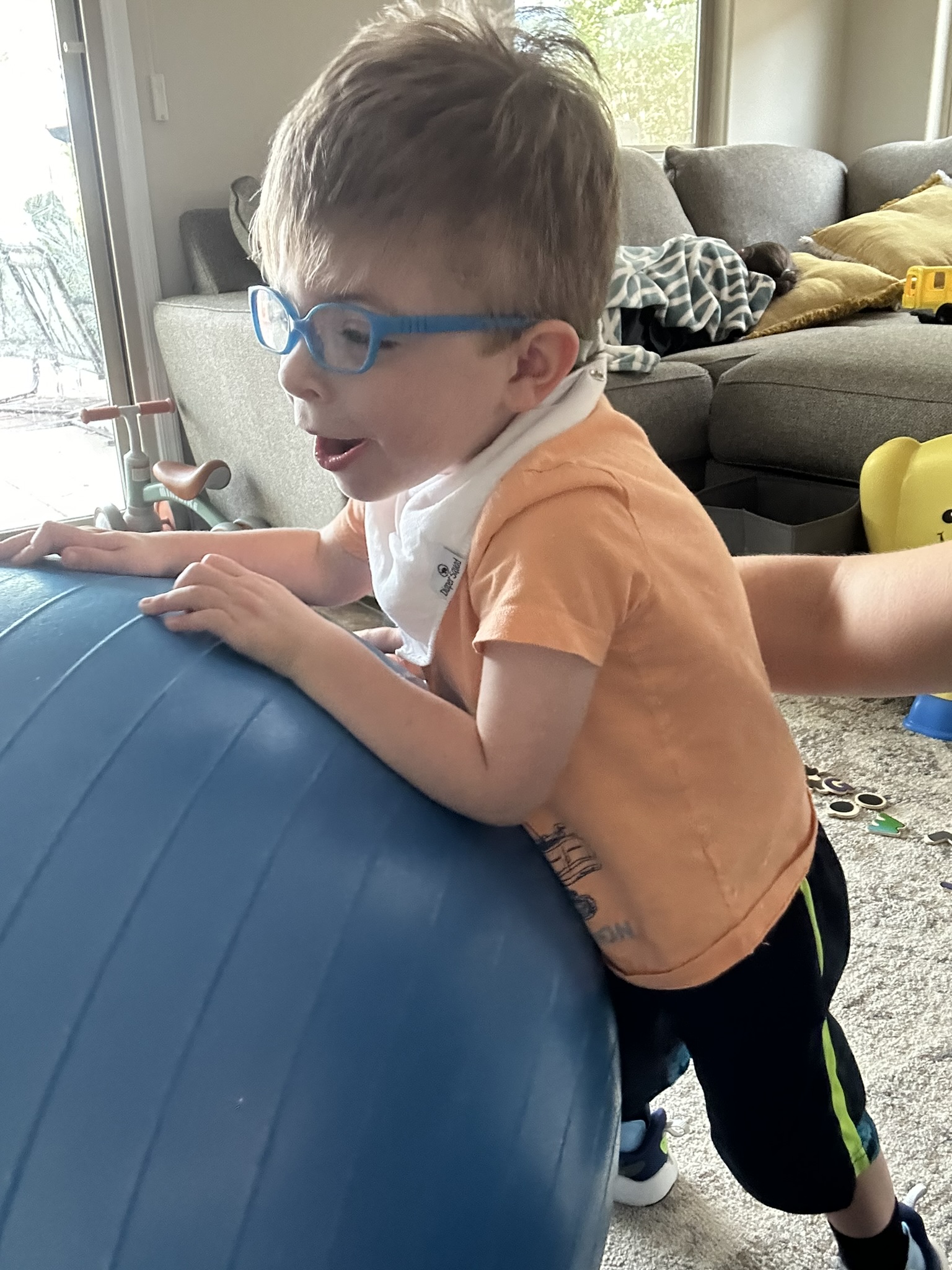
Hypotonia (low muscle tone)/ Floppiness
Hypotonia, defined by low muscle tone, is a condition that is defined by less than average muscular resistance when the muscles are moved passively. Children with this condition are generally referred to as 'floppy, flimsy, unaware of their bodies in space, weak, slipping through your hands when picked up, lazy' etc. They may be referred to as 'snuggle bugs' and allow their body to more or less melt into the furniture or person they are next to. They often assume postures in which they are hanging on their ligaments rather than using their muscles to engage in a more upright and engaged posture. Examples of this include open mouth posture, 'w' sitting, and leaning on furniture rather than sitting or standing upright. A person's muscle tone cannot change outright or permanently. Physical therapy and occupational therapy help children understand which muscles to activate and which postures will require strength rather than continually stretching out ligaments. Sometimes this is also addressed with orthotics.
Hypertonia (high muscle tone)/ Rigidness
Hypertonia, defined by high muscle tone, is a condition that is defined by more than average muscular resistance when the muscles are moved passively. Children with this condition are generally referred to as 'tight, rigid, unable to relax, pushing against you when held,' etc. Upon inspection, if their joints are frequently moved into an extended position, you may see skin irritation or redness in those areas, as the skin is unable to easily breathe. You may be constantly placing yourself or cushions behind your child when sitting or standing, as they are more likely to fall backwards than forward. A person's muscle tone cannot change outright or permanently. Physical therapy and occupational therapy help children understand which muscles to turn off vs. turn on and which postures will require allow them to relax. Sometimes this is also addressed with medication, orthotics and surgery depending on the intensity, age, interference with daily activities, and pain the child is experiencing
Cerebral Palsy (CP)Hemiplegia/ Monoplegia/Triplegia/Diplegia/ Quadriplegia
Cerebral palsy is a group of disorders that affects the nervous system that cause delays in several areas of the body. Many individuals with CP struggle with their bodies responding to what their brain is telling them, and can have physical limitations and restrictions as a result. Depending on which part of the brain is affected, the movement patterns can be more fluid-like or robot-like. Monoplegia means one limb is affected. Hemiplegia means that the left or right half of the body has been affected. Triplegia means that 3 limbs are affected. Diplegia means that the lower half of the body is more affected than the upper half of the body. Quadriplegia means all 4 limbs are affected. Physical therapy and occupational therapy address these conditions by helping the child understand their affected limb exists, how to use it rather than ignore it, bracing or splinting to keep it functional, recommending constraint induced movement therapy (CIMT), or working with the child pre/post surgery to help the limb(s) become more functional. Many times, children with cerebral palsy often have hypertonia, hypotonia, or mixed muscle tone that also affects their abilities to hold their bodies upright. If you are a caregiver for a child with cerebral palsy, we will help, regardless of their age.
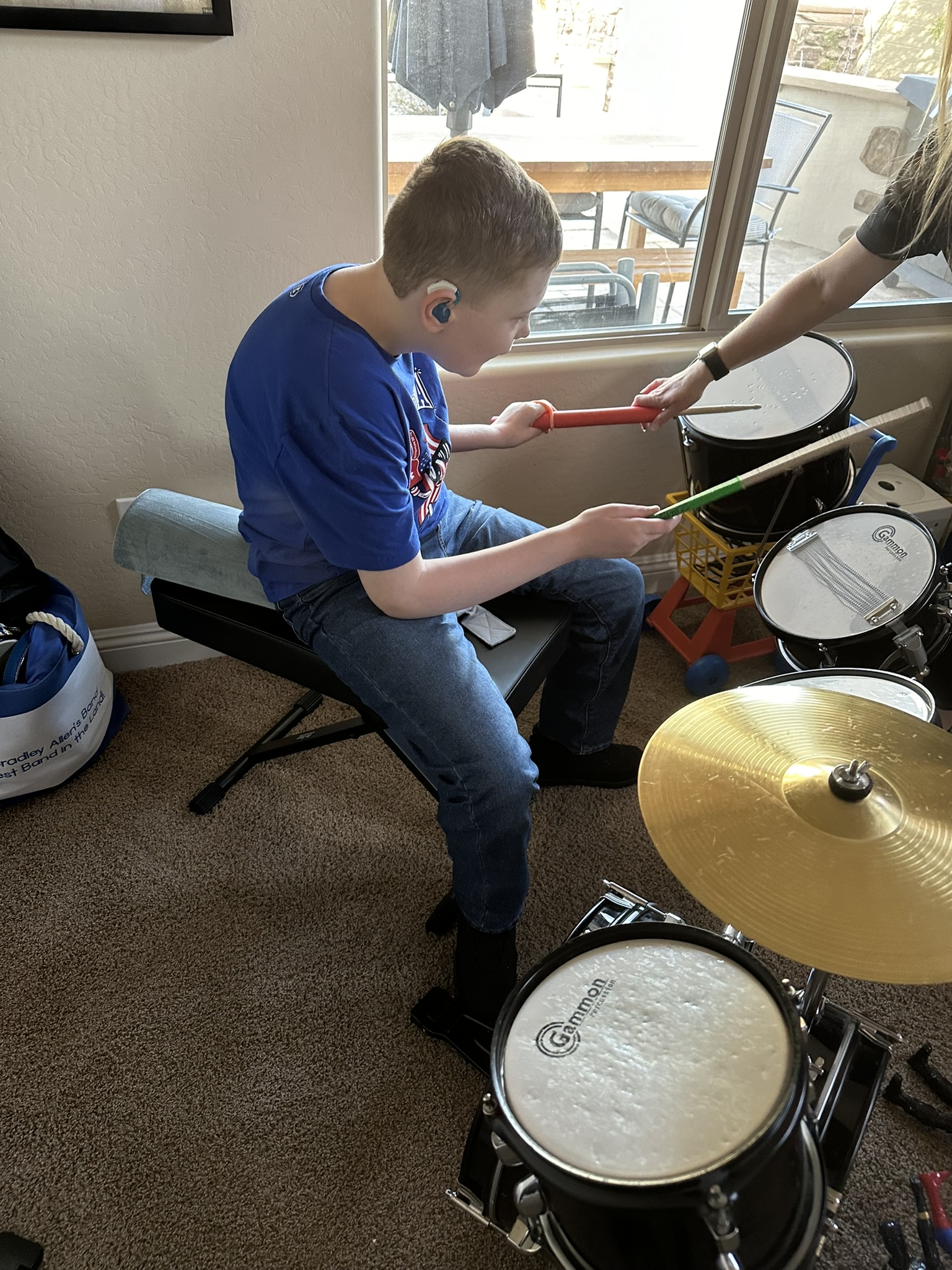
Autism (ASD), ADD/ ADHD +Associated Conditions
Autism, ADD, ADHD... These conditions have many overlaps in terms of their presentation, and difficulties with using their mind and body together to come up with the ideal result of how to move the body effectively. We often intervene with these conditions due to a lack of body awareness, atypical postures or movement patterns (w sitting and toe walking), frequent injuries due to falls or 'clumsiness,' and hypo- or hypertonia. Finding ways that your child with these conditions will succeed in a way that doesn't cause overwhelm is key.
Leg Length Discrepancy (LLD)
A leg length discrepancy is what it sounds like, when the legs are not the same length. This may cause a child to walk with a limp, trip, fall or stumble. Although each human body has a degree of asymmetry, if the leg length discrepancy is notable enough, it may cause the child to develop compensations in other parts of their body. This in turn can lead to pain, weakness, tightness and stiffness, leading a child to have an increased risk of falls and injuries. Sometimes it is necessary to utilize a lifted shoe and/ or undergo surgery in addition to physical therapy.
Weakness
Weakness is commonly seen with and without accompanying diagnoses in the physical and occupational therapy worlds. Weakness can be something that we are born with, or develop over time. As we become more sedentary and our lives become more automated, we are required to utilize our musculature less and less. If you've heard the phrase, 'if you don't use it, you lose it,' it does apply to our bodies as well. Yes, older children may often benefit from additional resistance such as weights or therabands, when strengthening their muscles. Babies, or children with extreme weakness, work on strengthening just through gravity eliminated and gravity enhanced positions, including the basic milestone progression of tummy time, sitting, reaching, crawling, standing, walking and carrying toys.
Tightness
Tightness often accompanies weakness. This can be due to overuse or underuse of a specific joint, muscle, or group of both in the body. Tightness often happens due to limited room to move in the womb (multiple fetuses). It can also occur due to positioning after the womb, such as being in the NICU and having limited movement due to lines and tubes. Tightness can also happen due to positioning that is practiced on a daily basis, such as sitting while playing with toys on the floor. This can also occur due to sitting at a desk in school with less time spent walking between classes or running at recess. Depending on the severity of the tightness, this may affect tendons, ligaments, joints and bones that can lead to asymmetry that ultimately makes it uncomfortable to move, sit or stand.
Scoliosis/ Kyphosis/ Lordosis
Scoliosis indicates a curved spine in our back. Scoliosis can be present from birth or can develop due to other diagnoses that pull on the muscles and bones asymmetrically. It can also develop due to trauma, such as a motor vehicle accident. Kyphosis and lordosis are often seen as a result of poorly practiced posture, such as having the head far forward while watching a screen, or sitting while reclining and not using our core to hold ourselves upright. Physical therapy can help encourage proper positioning and alignment through a variety of interventions. Additional specialists may be needed depending on the severity of the curvature.
Poor Posture
Poor posture is generally a combination of weakness, stiffness and tightness. It is sometimes paired with low muscle tone (hypotonia). Poor posture could be defined by kyphosis (rounding of the spine) with a forward head and rounded shoulders. It can also be more vague, such as wanting to lean or lay on furniture rather than sit in an upright position. Poor posture can be mistaken as apathy or laziness when there may be a true musculoskeletal or physiological reason causing it.


(Spastic) Paraplegias
Spastic paraplegias often affect the lower body more than the upper body and can be progressive, meaning they will become worse (more involved) with time. These conditions may limit a child from independently standing or walking. Physical and occupational therapy can help choose appropriate durable medical equipment (DME) to best utilize the independence a child currently has and/ or will develop, without taxing them from doing activities of daily living.
Hip Dysplasia (DDH)
Developmental hip dysplasia is when the hips are not properly aligned. This can be caused by the positioning of the fetus in utero, difficulties with delivery, a family history, or other anatomical malalignments. The femur inserts into the pelvis to create a stable joint for us to sit, stand and walk on in 'normal' anatomy. The hip(s) become(s) unstable in DDH and thus creates difficulties with mobility, range of motion, strength and ability to bear weight. This can be treated by PT in conjunction with monitoring, a Pavlik harness, surgery and/or a spica cast from an orthopedic physician.
Brachial Plexus Injury (BPI)
A brachial plexus injury is defined as injury to the nerves and surrounding tissues in the shoulder region that cause difficulties with posture, alignment and use of that upper extremity (arm). This could cause the arm to droop to the side, as the child may not fully feel it, or experience numbness/ pins and needles. It can also cause difficulties with weight bearing through the arm, making tummy time, hands and knees or crawling difficult. This could be caused by a variety of factors, and sometimes does also require a visit with a neurosurgeon.
Down Syndrome/ Trisomy 21
Down syndrome is a genetic condition that is caused by an extra chromosome (21), affecting some or all of the cells. Down syndrome is associated with low muscle tone (floppiness), ligamentous laxity in the joints, and flat feet. It has several other characteristics associated with it as well, including developmental delay. Due to this condition affecting all areas of development, there is a separate milestone chart for children with down syndrome, so as not to be compared to typical peers.
Tip Toe/ Idiopathic Toe Walking (ITW)
Toe walking is defined by a lack of heel contact, or a shortened time that the heel is in contact with the ground, when walking. It can appear like a person is 'bouncing' on the balls of their feet, and otherwise described as a 'controlled fall.' Toe walking can occur due to a variety of reasons, and is broken into 3 categories, including musculoskeletal, sensory, and neurological. Depending on the subtype of toe walking that your child has, this can be treated by physical therapy, occupational therapy, a variety of both, and other specialists. Additional equipment or surgeries may be necessary depending on the intensity of the toe walking and the flexibility of the ankle joint and other foot and toe bones. It is extremely important that you find a pediatric physical therapist and occupational therapist who is experienced in idiopathic toe walking in order to understand the appropriate interventions needed to truly target the toe walking.
Cortical Visual Impairment (CVI)
CVI is a condition in which the brain is unable to process what the eyes can see, or a disconnect between the eyes and the brain. As >80% of our sensory input is due to our vision, this generally is associated with delayed milestones. Physical and occupational therapy can help your child learn how to navigate their environments safely and find adaptations to make them more independent. This can include sensory integration techniques, hand-eye coordination, and trying out assistive devices to help the child crawl, sit, stand and walk.
Rhett Syndrome
Rhett syndrome is a genetic disorder that involves many aspects of development, often causing regressions. In physical therapy and occupational therapy sessions, we focus on ways to limit energy uses focus on energy conservation. We also improve independence with a variety of tools/ positioning devices or durable medical equipment. We aim to enhance endurance while also focusing on ways to reduce the workload of the caregivers in order for them to reduce their risk of injury with transfers.
Pediatric Cancer
Cancer can show up with a variety of side effects in children and adults alike. Sometimes they can cause delays, others a change in muscle tone, and others a deficiency in strength and endurance. Any aspect of the body that is physically involved in pediatric cancer can be addressed with physical therapy and occupational therapy.
Sever Disease
Sever disease is a condition in which the back of the heel on the foot becomes inflamed and painful, making it difficult to walk and run. Physical therapy can work on pain management and activities to reduce the swelling in order to return your child to what they love the most: play!


Retained Primitive Reflexes
Primitive reflexes are involuntary movements that are first practiced by the fetus in utero that are meant to help with the birthing process and exploration as an infant. These are movements that are pre-conditioned (reflexive) for the child to utilize rather than voluntary, and seen as a response to a stimulus. As the child's nervous system matures, these reflexes are expected to 'integrate,' or rather become voluntary rather than pre-selected. Signs that your child may have unintegrated reflexes include awkward or clumsy movements, the body doing something 'opposite' of what you would expect based on the stimulus, or heavily locking out joints or leaning on joints when doing 'basic' movements. They may avoid ball sports, be considered clumsy, or become easily frustrated with physical tasks. Physical therapy and occupational therapy can help rewire the brain-body connection to change these movement patterns from involuntary to intentional and helpful.
Gait Abnormalities
Gait is the medical term used to describe how a person walks. A gait abnormality signifies that a child is walking in a manner that is atypical. This could be due to any of the conditions listed above, including scoliosis, hip dysplasia, leg length discrepancy, tightness, weakness, or atypical muscle tone. Physical therapy can address the reason behind the abnormality and also work on improving the child's symmetry when standing and walking.
Chromosomal Abnormalities & Genetic Disorders
Chromosomal and genetic abnormalities can play a role in a child's developmental milestone progression. Depending on the condition that the child has, there may be physical, emotional or sensory difficulties associated with it. Physical and occupational therapy can work on the physical development, play skills, emotional development and adaptive/ self help skills. We can also recommend different pieces of durable medical equipment (DME) to improve your child's independence and alignment as a result of their genetic condition.
Pre-Surgical Intervention/ "Prehab"
Prehab is what an individual would do in order to prepare for a surgery. Generally, it is best to become the most independent and functional prior to undergoing a surgery or another invasive procedure, such as a muscle or tendon lengthening procedure. This could also be due to a torn ligament due to a traumatic event, like a sports injury or car crash. The goal is to limit the time spent recovering after surgery by learning various movement techniques, improving strength and mobility, and increasing independence in physical therapy and occupational therapy.
Post-Surgical/ "Post-op"
Seeing a child after surgery would also be referred to as post-operative physical or occupational therapy. After surgery, children may experience pain, limited movement, and difficulty with everyday tasks. Physical therapy helps restore strength, mobility, and range of motion, while occupational therapy supports the child in regaining independence with tasks like dressing, eating, and school activities. PT and OT focus on safe movement and gradual return to normal activities while following precautions or restrictions set in place by the orthopedic surgeon. Pain management techniques as well as caregiver education are heavily covered in these sessions. Both therapies are essential for a smooth recovery and to help children regain their physical abilities and independence as quickly as possible.
Obesity
Obesity is a condition characterized by excessive body fat that can lead to various health complications, generally resulting in decreased mobility. Individuals with obesity may experience difficulties with physical activity, balance, and performing daily tasks. Physical therapy can help by improving strength, endurance, and flexibility through targeted exercises, while also promoting weight management. Occupational therapy can assist with adapting daily routines and improving overall functionality in daily activities. Both therapies work together to support weight loss, reduce strain on joints, and improve quality of life by focusing on both physical and functional aspects of the condition.
Deconditioning
Deconditioning in children happens when they become less active due to illness or injury, leading to weaker muscles and less stamina. It can result in decreased muscle strength, endurance, balance, and coordination, affecting one’s ability to perform everyday activities. Physical therapy plays a key role in restoring strength, endurance, and flexibility through gradual, individualized exercise programs. Occupational therapy focuses on helping individuals regain functional independence by adapting tasks and improving energy.
Spina Bifida
Spina Bifida is a birth defect in which the spinal cord and surrounding vertebrae do not develop properly, leading to varying degrees of mobility impairment, sensory loss, and bladder/bowel dysfunction. Children with spina bifida may experience difficulty with walking, coordination, and performing daily tasks. Physical therapy is crucial in improving mobility and strength and preventing complications such as joint deformities. Physical therapy can include exercises to enhance walking ability, posture, and balance. Occupational therapy focuses on helping individuals develop skills needed for daily living, such as dressing, bathing, and managing school or work tasks. Both therapies aim to maximize independence and functional capacity, helping individuals with spina bifida live their lives to the fullest.
Muscular Dystrophies (DMD)
Muscular Dystrophies, including Duchenne Muscular Dystrophy (DMD), are a group of genetic disorders that lead to progressive muscle weakness and loss of muscle mass. Individuals with MD may experience difficulty with movement, posture, and daily activities as their condition advances. Physical therapy helps by focusing on strengthening remaining muscles, improving flexibility, and preventing contractures (shortening of muscles and tendons). PT also works to maintain mobility and promote the use of adaptive devices, such as wheelchairs or braces, to enhance independence. Occupational therapy assists by improving fine motor skills, teaching energy conservation techniques, and adapting activities of daily living to maintain autonomy for as long as possible. Early intervention from both PT and OT can help slow the progression of disability and improve the overall quality of life for individuals with muscular dystrophy.

Clumsiness
Clumsiness, sometimes as a result of the condition Developmental Coordination Disorder (DCD), is a condition that affects coordination and motor skills, leading to difficulties with tasks that require fine and gross motor coordination, such as writing, tying shoelaces, or catching a ball. Children and adults with DCD often experience frustration and low self-esteem due to their challenges. Physical therapy is used to improve motor planning, balance, coordination, and strength through structured exercises and activities. Occupational therapy focuses on helping individuals improve their fine motor skills and perform daily activities, such as dressing, eating, and schoolwork, more effectively. It also targets coordination, like physical therapy. Both therapies can provide strategies for managing challenges and building confidence in performing everyday tasks.
Apraxia
Apraxia is a neurological disorder where individuals have difficulty planning and coordinating the movements required for voluntary actions. In cases of motor apraxia, individuals may struggle to perform purposeful movements, such as brushing their teeth or buttoning a shirt. PT can help with motor coordination exercises to improve voluntary movements and build strength in affected muscles. OT is essential in helping individuals develop or regain the ability to perform daily tasks through adaptive techniques, compensatory strategies, and tools that facilitate easier performance of activities. Speech therapy may also be involved for individuals with speech apraxia to improve communication. Through coordinated care, PT and OT aim to enhance functional independence, safety, and overall quality of life.
Sensory Processing Disorders (SPD)
Sensory Processing Disorder (SPD) occurs when the brain has difficulty interpreting and responding to sensory input. Individuals with SPD may over-respond or under-respond to sensory stimuli such as touch, sound, light, or movement. This can impact daily activities and social interactions. Occupational therapy (OT) can help children and adults with SPD by providing strategies and sensory integration techniques to improve their ability to process and respond to sensory input in a more manageable way.
Emotional/State Regulation
Emotional or state regulation refers to the ability to manage and respond to emotions in a healthy way. When this regulation is impaired, a child may struggle to cope with frustration, anxiety or transitions, and may have difficulty controlling their emotional reactions. This can result in behavioral challenges at home or school. Support in the form of therapy, social skills training, or behavioral strategies can be beneficial for helping children learn self-regulation techniques. Our occupational therapy interventions can help address difficulties with emotional and state regulation difficulties.
22Q (DiGeorge Syndrome)
22Q (also known as DiGeorge Syndrome) is a genetic disorder caused by a deletion on chromosome 22. It can lead to a variety of physical, developmental, and health-related challenges, such as heart defects, immune system issues, learning difficulties, and speech delays. Early intervention with physical and occupational therapy is important, as therapies and medical support can help manage symptoms and promote development. Families may also benefit from a larger team of specialists, including genetic counselors, cardiologists, and speech therapists.
Concussion/TBI (Traumatic Brain Injury)
A concussion is a type of mild traumatic brain injury (TBI) that can occur after a blow to the head. Symptoms may include headaches, dizziness, confusion, or difficulty concentrating. While many people recover with rest and time, persistent symptoms or more severe injuries may require medical attention and rehabilitation. Physical therapy (PT) and occupational therapy (OT) can assist in managing post-concussion symptoms and help individuals return to daily activities safely.
Executive Dysfunction
Executive dysfunction refers to difficulties with skills that help us plan, organize, problem-solve, and manage time. Children or adults with executive dysfunction may struggle with tasks such as following through with plans, staying on task, or managing multiple responsibilities at once. This can impact academic performance and daily life. Cognitive therapy, behavioral strategies, and accommodations at school or work can be implemented through skilled occupational therapy and prove to be beneficial in helping to strengthen these skills.
Visual Processing Disorders
Visual processing disorders occur when the brain has trouble interpreting visual information, despite having normal vision. Individuals may struggle with reading, writing, or recognizing visual patterns and shapes. This can affect academic performance and daily tasks that require visual discrimination, such as catching a ball or reading a map. Occupational therapy (OT) can help children and adults improve their visual processing skills through specific exercises and strategies.

Follow Us
Follow Us
Confident Beginnings is our month-by-month development coaching program for your baby's first 18 months. It bridges the gap between your questions and rushed pediatrician appointments.
Confident Beginnings is available for families worldwide for parents of children 0-18 months old.
Services
More
Contact Us
Monday - Friday: 8:00 am - 5:00 PM
8603 E. Royal Palm Rd. #120, Scottsdale, AZ 85258
In home and virtual pediatric PT + OT services in Scottsdale, AZ + surrounding areas.
© Copyright 2026. Moving and Grooving Physical Therapy. All rights reserved. Sitemap. Privacy Policy